Public health experts call this the respiratory virus season, and the latest statistics have been swinging up as they do every year.
Influenza (flu), RSV, and COVID are all on rising trends nationally and here in King County. (RSV is respiratory syncytial virus, a particular threat for infants and seniors.)
Two of the three — RSV and flu — have reached officially designated transmission alert levels. Public Health — Seattle & King County (PHSKC) monitors emergency department visits as a reliably reported source of lab test data for each of the three respiratory ailments. You can track the reports here.
RSV: Transmission alert level reached
Flu: Transmission alert level reached
COVID: Still below transmission alert level
Why is a transmission alert important? It’s a protocol that alerts healthcare facilities when community spread of one of the three respiratory viruses has increased to a high-risk level. The system tracks the percentage of people who test positive for one of the three respiratory viruses during emergency room visits, and an alert is posted when positive tests get above a predetermined level.
The Northwest Healthcare Response Network (NWHRN) has set the alert levels for the organization’s healthcare facility members. NWHRN recommends actions for facilities to take in response to an alert. For example, MultiCare hospitals have reinstated indoor masking policies in King, Kitsap, and Pierce counties. Seattle Children’s is doing the same. UW Medicine has started to require health care staff to mask up in patient care spaces.
Why is Respiratory Virus season happening now?
People used to call fall and winter the flu and cold season. It happens every year because:
- It’s cold, so people are gathering indoors, rather than having outdoor picnics where there’s less chance of virus spread.
- People are gathering and traveling for holiday festivities, and when people come together, that’s an environment to spread infections.
- It’s not just flu and colds anymore. COVID is still with us, and there’s more awareness and concern about RSV.
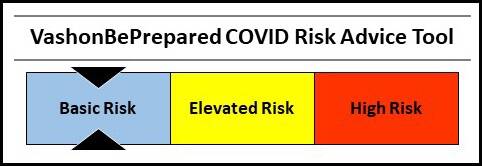
Vashon COVID Risk Level: Basic
Our weekly VashonBePrepared COVID Risk Advice Tool aggregates data from our two-county exposure area (King and Pierce). The primary metric evaluated by the Vashon Medical Reserve Corps is the COVID hospitalization rate.
Unlike home tests, hospitalizations are reliably reported to public health agencies and can accurately be tracked for trends. Also, the hospitalization rate folds the element of disease severity into the risk assessment.
Remember, basic risk is not zero risk.
Some Easy Common-Sense Ways to Play It Safe
Fortunately, the basic common-sense steps we learned to take at the height of the pandemic also work well to prevent spread of RSV and flu.
- If you wear a mask, as you have done for COVID, you also significantly reduce the chances of getting flu or RSV.
- Avoid indoor crowds. It’s called a respiratory virus for a reason. Infected people exhale infected air. If you are breathing their air, you could become infected. Often, you have no way of knowing if someone is infected, because they may not have obvious symptoms.
- If you decide to host an indoor event, try to improve the air quality. For example, for a dinner party, run air purifiers in the dining room and consider opening nearby windows.
- Be extra vigilant if you are susceptible because your immune system is weakened or you have other risk factors.
- Get vaccinated. There are updated vaccines for all three of the concerning diseases: COVID, flu, and RSV. If you have questions about the vaccines, ask your pharmacist, or physician, or call the Vashon Medical Reserve Corps hotline at 844- 469-4554.
- Avoid exposure to people who are sick. And if you have symptoms, stay home until your fever is gone and you are feeling substantially better.
- Test for COVID with a home test when cold symptoms appear, and again 48 hours later. If you test positive, isolate for at least 5 days and until you test negative. Also check in right away with your doctor about treatment, even if your symptoms are initially mild.
“I Already Had COVID, So I’m Good, Right?”
We know that prior COVID infections provide short-term protection against reinfection, but many people have had second (and third!) COVID infections. An earlier infection is not an invincible shield.
More importantly, there’s new evidence that having COVID more than once increases the risk that you will get long COVID. A 3-year study of 138,000 veterans who had COVID reinfections showed that each additional infection contributes additional risk of long COVID (bit.ly/LongCOVIDrisk).
Fatigue, brain fog, muscle pain, shortness of breath, gut problems, heart rate disruptions — all these have been described as long COVID symptoms. Long COVID symptoms can linger for months or even years after your tests show negative for COVID.
These long-lasting and sometimes severe long COVID symptoms are good reasons to get caught up on the COVID vaccine and help protect ourselves from severe COVID infections.
Get Your Free Home COVID Tests
If you haven’t already requested them, don’t forget to get your four free additional COVID tests. Go to COVIDtests.gov and order now.
The federal government reopened the free test program last month so you can get four more tests, even if you already received four. If you didn’t order any when the free test program first came out, you can get eight tests.